Parathyroid Hormone (PTH): The Unsung Regulator of Bone Health
Most people have heard of calcium or vitamin D. But Parathyroid Hormone (PTH)? It rarely gets mentioned — yet plays a central role in regulating your bones.
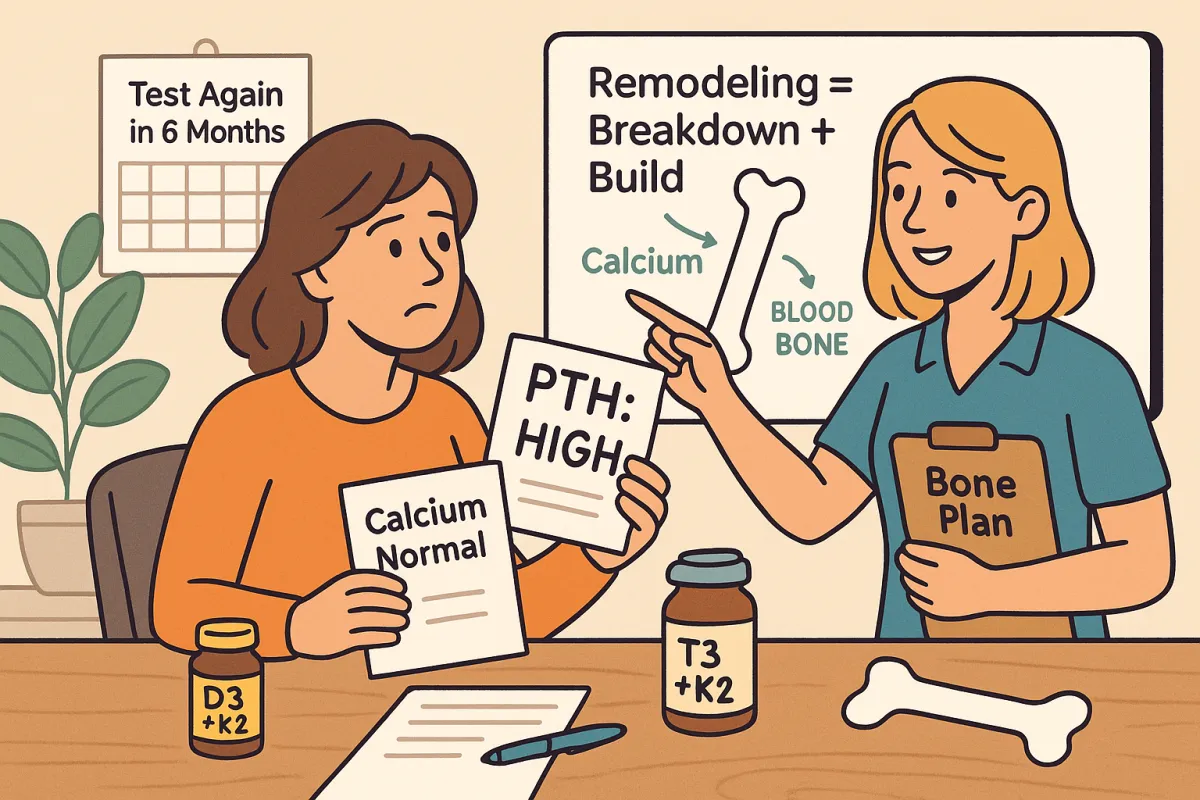
If your PTH is out of balance, you could be losing bone even if your calcium or vitamin D levels look okay. Let’s unpack what it is, why it matters, and what you can do.
🔍 What is PTH?
PTH is a hormone released by your parathyroid glands, which are four tiny glands located behind your thyroid.
Its main job? Regulating calcium levels in your blood — and it does this by:
Pulling calcium out of your bones if your blood levels drop
Reducing calcium loss through urine
Triggering vitamin D activation, which helps your body absorb more calcium from food or supplements
In simple terms: PTH acts like a calcium traffic controller. It keeps things steady in your bloodstream — often at the expense of your bones.
🧠 Why It Matters for Your Bones
Here’s the problem:
If your PTH stays high for too long, it constantly pulls calcium out of your bones, weakening them over time.
This can happen even if:
You’re taking calcium supplements
Your vitamin D looks “normal”
You don’t have any symptoms
Some people have primary hyperparathyroidism (when the gland itself goes rogue), but many more have “secondary” PTH elevation due to low vitamin D, poor calcium intake, kidney issues, or medication side effects.
🧪 What to Test
A full hormone picture should include:
PTH
Vitamin D (25-OH D3)
Serum calcium
Optional: kidney markers or magnesium, depending on symptoms or history
These tests can help reveal if your body is leaching calcium from your bones to keep blood levels stable — even if other markers look fine.
💡 Did You Know?
Up to 10% of older adults — especially postmenopausal women — have abnormal parathyroid hormone (PTH) levels, and most don’t even know it.¹
That’s because PTH issues rarely cause symptoms early on — you could have suboptimal regulation for years before it shows up in a bone scan.
This makes periodic testing a smart move, especially if you:
Are postmenopausal
Have a history of low vitamin D
Are on calcium or bone medications
Have digestive or kidney issues
🛠️ What If It’s Too High?
If your PTH is elevated, it means your body is actively breaking down bone to keep blood calcium stable. That doesn’t mean your calcium intake is low — but it might not be getting absorbed properly.
Possible causes include:
Low vitamin D (very common)
Poor calcium intake or absorption
Long-term PPI or steroid use
Kidney function issues
Parathyroid tumor (rare)
You’ll need help from your doctor to rule out or confirm the root cause. But in the meantime, here are strategies that may help:
✅ Smart Strategies:
Get enough bioavailable calcium (500 mg max per dose)
Pair with vitamin D3 and K2 to improve absorption and direction
Test your magnesium status — it’s required for proper PTH control
Eat a nutrient-dense, anti-inflammatory diet
Avoid very low-calorie diets that suppress hormone production
🔽 What If It’s Too Low?
Low PTH can mean your bones aren’t getting enough stimulation to remodel — or it may signal issues with your parathyroid gland function. In some cases, over-supplementing with calcium or having high vitamin D can suppress PTH.
That’s why PTH needs to be interpreted in context — more isn’t always better, and neither is less.
❗ A Note on Supplements
If you're taking calcium supplements and your PTH goes down, that might look like a win. But be careful:
A lower PTH doesn't always mean your bones are rebuilding properly.
You may be “flooding” your system with calcium, but if it’s not being directed into bone — or if remodeling is suppressed — you could end up with calcium in the wrong places, like soft tissue or arteries.
This is why vitamin K2, magnesium, and D3 are such helpful teammates. They help make sure calcium ends up in the bone — and nowhere else.
🧭 Final Thought
PTH is one of the most under-checked and under-discussed pieces of the bone health puzzle.
And while most people focus on calcium or vitamin D, your PTH may be the real driver of bone loss — or a clue to deeper issues.
Good news? You can test it. You can track it. And you can improve it.
Start by getting a full panel, and use your Bone Audit report to guide the next steps.
